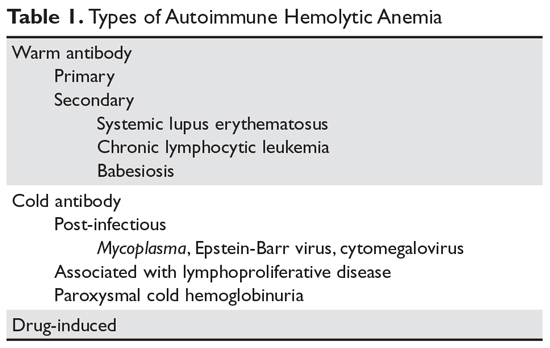
Autoimmune hemolytic anemia is caused by autoantibodies that react with red blood cells at temperatures 37 C warm antibody hemolytic anemia or 37 C cold agglutinin disease. These rare conditions occur when antibodies.
Autoimmune hemolytic anemia AHA is a group of disorders where your immune system mistakenly destroys your own red blood cells RBCs.

What causes autoimmune hemolytic anemia. This eventually causes red blood cells to be prematurely destroyed hemolysis leading to anemia and other associated signs and symptoms. Consequent complement activation can impact the clinical picture and is an emerging target for therapeutic approaches. Autoimmune hemolytic anemia AIHA or immune hemolytic anemia happens when the immune system does not work properly.
Autoimmune haemolytic anaemia associated with COVID-19 infection. The patients own antibodies are directed against antigens on their own red blood cells resulting in. Destruction of red blood cells by autoantibodies.
Immune causes of hemolytic anemia from nonimmune causes. This causes a drop in the number of red blood cells leading to hemolytic anemia. Autoimmune haemolytic anaemia associated with COVID-19 infection.
Acquired hemolytic anemia is not something you are born with. Autoimmune haemolytic anaemia associated with COVID-19 infection. Autoimmune hemolytic anemia AIHA is a decompensated acquired hemolysis caused by the hosts immune system acting against its own red cell antigens.
Autoimmune haemolytic anaemia associated with COVID-19 infection. Autoimmune hemolytic anemia AIHA occurs when your immune system makes antibodies that attack your red blood cells. Cold agglutinin disease can be primary unknown cause or secondary due to an underlying condition such as an infection another autoimmune disease or certain cancers.
It mistakes red blood cells for unwanted substances and attacks them causing. Cancers including chronic lymphocytic leukemia and non- Hodgkins lymphoma. Some of these are.
Other diseases and medications can also cause autoimmune hemolytic anemia. When a patient presents with anemia a stepwise approach should be followed. The direct antiglobulin direct Coombs test establishes the diagnosis and may suggest the cause.
Autoimmune Hemolytic Anemia AIHA is characterized by antibody-induced erythrocyte destruction. Immune Hemolytic Anemia AUTOIMMUNE HEMOLYTIC ANEMIA AIHA is caused by autoantibody-mediated destruction. Hemolytic anemia is a disorder in which the red blood cells are destroyed faster than they are made.
Some of these are. You develop the condition later. One of the most severe forms of hemolytic anemia is the kind caused by receiving a red blood cell transfusion of the wrong blood type.
Every person has a. Autoimmune hemolytic anemia can also be caused by or occur with another disorder such as systemic lupus erythematosus lupus or a lymphoma and it can be due to the use of certain drugs such as penicillin. Inherited hemolytic anemia means that parents pass the gene for the condition on to their children.
Hemolysis is usually extravascular.
This disease represents no threat to human health. Especially lice fluke worms skinlivergut etc.
 Fall And Winter Health Problems In Cow Calf Herds
Fall And Winter Health Problems In Cow Calf Herds
Also asked what are the symptoms of leptospirosis in cattle.

What causes anemia in cattle. Its just that a heavy worm load is one thing that can cause anemia which in turn causes bottle jaw. So it isnt necessarily caused by worms. Theileria parva in cattle and Cytauxzoon in cats are associated with a non-regenerative anemia potentially due to infection of erythroid progenitors with Theileria and concurrent anemia of inflammatory disease with Cytauxzoon.
The reason for the leukocytes neutrophil and. Ketosis cause the cows to have low blood glucose concentration. Early stage of Lactation If your cattle especially dairy cows shows loss of appetite in their early lactation it can be caused of bovine ketosis and indigestion.
In this study cause of anemia in the mild and moderate forms was not related to the hemorrhagic hemolytic chronic diseases bone marrow factors but nutritional aspects could still be the major criteria. In the present study plasma protein increased with age and for calves with mild to moderate anemia was 8 and 714 mgdl respectively. The husbandry of calves in this area has already been described Sharman 1954.
Winter anaemia usually recovers within 1 month after turnout to good pasture. Immune-mediated hemolytic anemia is treated with immunosuppressive drugs. Haemoglobin levels usually rise from Apr to Nov and fall from Nov to Apr.
Immune-mediated destruction is the most common cause in dogs although infections tumors and other causes also occur. The progressive loss of weight anemia weakness and anorexia are among the symptoms reports the British Department for Environment food and Rural Affairs-Defra. Anemia caused by hemorrhage or hemolysis is typically regenerative.
Clostridium haemolyticum causes bacillary hemoglobinuria BH an infectious and usually fatal disease that occurs mostly in cattle which is clinically characterized by jaundice hemoglobinuria and anemia. Bovine ketosis is a disorder which happens in cattle exceed energy intake hence there is negative energy balance. Hemolytic anemia is caused by blood parasites toxins electrolyte imbalances hypoosmolality 71922 or autoimmune reactions.
Hemorrhagic anemia can be caused by ectoparasites or parasites of the gastrointestinal system hemorrhagic bowel syndrome abomasal ulcers vena cava thrombosis as well as from the genitourinary. 40 In cattle common causes for hemolysis include unsuitable food and toxic plants such as cabbage Brassica spp onions Allium cepa rye grass Lolium spp or red maple Acer rubrum. Anemia caused by decreased erythropoietin or an abnormality in the bone marrow is nonregenerative.
Protozoal bacterial viral fungal. Farmers must slaughter all infected cattle. Bovine Anemia-Theileria Benign theileriosis is a tick-borne disease caused by intracellular blood parasites belonging to the Theileria orientalis group BATOG.
Redwater disease in cattle is a febrile tick-borne disease caused by one or more intra-erythrocytic protozoan parasites of the genus Babesia which is generally characterized by extensive erythrocytic destruction resulting in anemia hemoglobinuria jaundice occasionally CNS involvement and death in severe cases. When leptospirosis associated with nonhost-adapted Lepto serovars occurs in calves the result is high fever anemia red urine jaundice and sometimes death in three to five days. The rearing system is characterized by a large daily intake of milk and the intake of solid.
Other types are treated by addressing the underlying cause. Bottle jaw is really just a manifestation of anemia where fluid accumulates in the low point of the head. 27192150 Microorganisms infecting ruminant RBCs.
To date the disease has been found in Australia in Victoria Queensland and. The trematode Fasciola hepatica has been commonly reported as the main predisposing factor that triggers this condition. Anemia caused by hemorrhage or hemolysis is typically regenerative.
Anemia caused by decreased erythropoietin or an abnormality in the bone marrow is nonregenerative. Our experiments have been carried out to find whether in the herds of beef cattle of north Scotland anaemia induced by Fe deficiency was a practical problem. Low qualityintake of winter feed.
In older cattle the initial symptoms such as fever and lethargy are often milder and usually go unnoticed. Hemolytic anemia results from loss of RBCs. Skin lesions and tumor formation in various organs such as intestines liver and lymph nodes can also happen.
Another option is surgery to remove the spleen called a splenectomy. The more commonly used treatments along with their.
 Transition From Chronic Relapsing Autoimmune Hemolytic Anemia Aiha Download Scientific Diagram
Transition From Chronic Relapsing Autoimmune Hemolytic Anemia Aiha Download Scientific Diagram
This is because of significant differences in the rates of hemolysis and associated diseases and because there is considerable clinical heterogeneity.
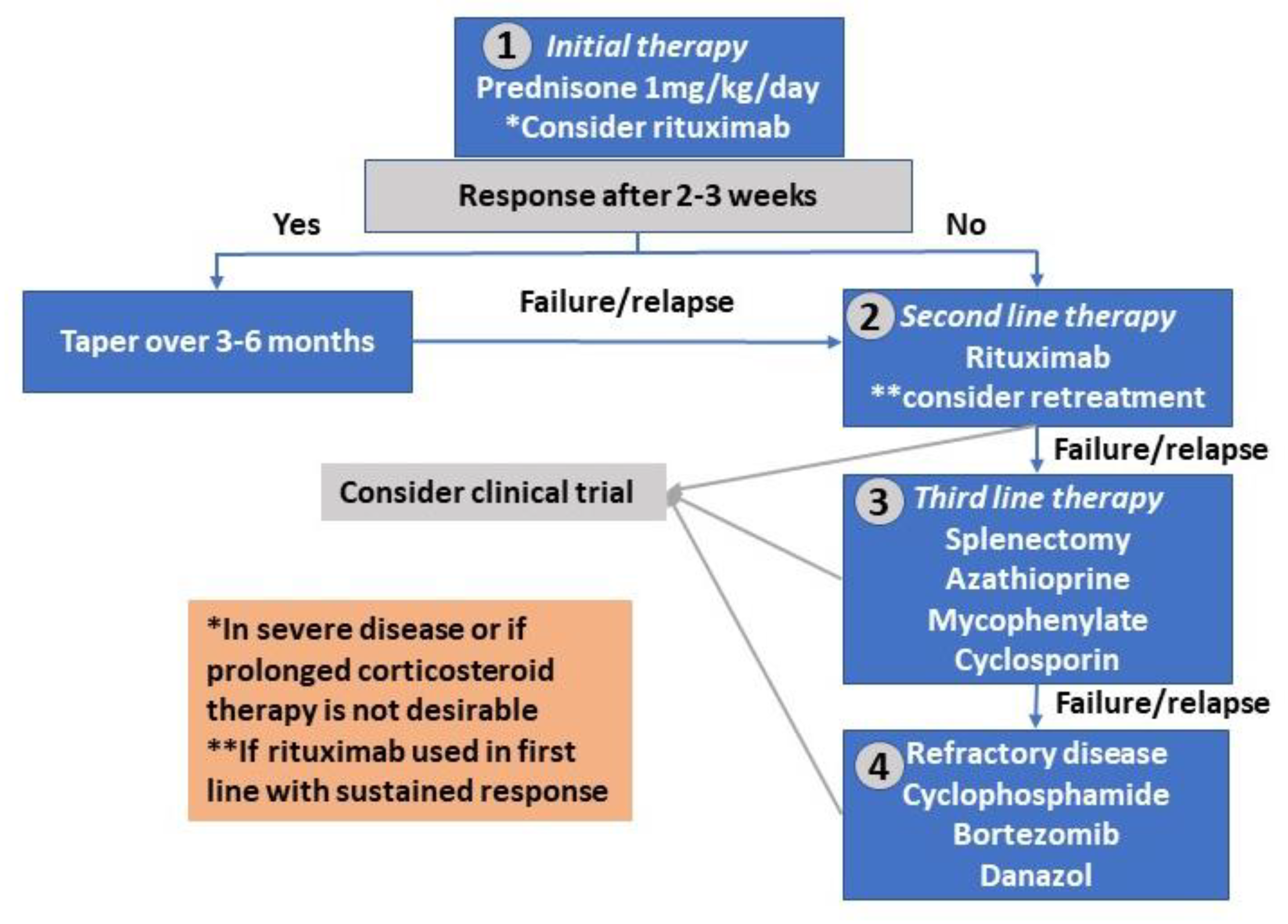
How i treat warm autoimmune hemolytic anemia. Microangiopathic hemolytic anemia MAHA refers to a subgroup of hemolytic anemia where there is fragmentation and hemolysis due to damage of erythrocytes in the small blood vessels. Primary warm antibody autoimmune hemolytic anemias respond well to steroids but most patients remain steroid-dependent and many require second-line. Warm AIHA due to antibodies that are active at body temperature is the most common type of AIHA.
Further evidence of hemolysis may include a reticulocytosis raised lactate dehydrogenase LDH low or. This is because of significant differences in the rates of hemolysis and associated diseases and because there is considerable clinical heterogeneity. In addition there is a lack of clinical trials required to refine and.
Daratumumab in life-threatening autoimmune hemolytic anemia following hematopoietic stem cell transplantation. Treatment decisions should be based on careful diagnostic evaluation. Treatment depends on the type of antibody causing the anaemia.
Autoimmune hemolytic anemia is a heterogeneous disease with respect to the type of the antibody involved and the absence or presence of an underlying condition. Antibody-dependent cell-mediated cytotoxicity by macrophagesactivated lymphocytes occurs in the lymphoid organs and spleen extravascular hemolysis. In one study warm AIHA represented 703 percent of the cases of AIHA that were encountered.
We combined these results with a review of 36 cases of AIHA treated with IVGG reported in the literature. Until now treatment of primary autoimmune hemolytic anemia of the warm type wAIHA is primarily based on immunosuppression. Autoimmune hemolytic anemia AIHA is an uncommon entity that presents diagnostic prognostic and therapeutic dilemmas despite being a well-recognized entity for over 150 years.
A high-dose of these drugs may be recommended initially followed by a gradual reduction tapering of the dose over the next few weeks or months. This topic reviews the evaluation and management of warm AIHA in adults. However many patients do not respond adequately to treatment and treated patients may develop severe side effects due to uncontrolled mixed andor long-lasting immunosuppression.
Antibody-dependent cell-mediated cytotoxicity by macrophagesactivated lymphocytes occurs in the lymphoid organs and. Antibody-dependent cell-mediated cytotoxicity by macrophagesactivated lymphocytes occurs in the lymphoid organs and spleen extravascular hemolysis. The ability of the bone marrow BM to compensate determines clinical.
Autoimmune hemolytic anemia AIHA is an uncommon entity that presents diagnostic prognostic and therapeutic dilemmas despite being a well-recognized entity for over 150 years. How I treat warm autoimmune hemolytic anemia. Similarly DAT negativity is not essential with controlled hemolysis.
If hemolysis continues that is well compensated after prednisone tapering starting a second-line treatment may not be necessary. Antibody-dependent cell-mediated cytotoxicity by macrophagesactivated lymphocytes occurs in the lymphoid organs and spleen extravascular hemolysis. Initial medical treatment consists of prednisone.
Erythropoietin may improve anemia in patients with autoimmune hemolytic anemia associated with reticulocytopenia. Corticosteroids and immunoglobulins are two commonly used treatments for warm antibody AIHA. Warm autoimmune hemolytic anemia wAIHA is caused by increased erythrocyte destruction by IgG autoantibodies with or without complement activation.
Not all people with warm type autoimmune haemolytic anaemia will need treatment but for those who do the first treatment is usually steroids. The ability of the bone marrow BM to compensate. Sixteen clinical variables were examined to determine associations.
Or 3 intolerance to a currently effective treatment. Rituximab is an artificially. Warm autoimmune hemolytic anemia AIHA is the most common type of AIHA.
It is characterized by the presence of red cell fragments or schistocytes on blood film review. Intravenous immunoglobulin G IVIG has been used for patients with AIHA but only a few patients have responded to this treatment and. Autoimmune hemolytic anemia AIHA is caused by autoantibodies that react with self red blood cells RBCs and cause them to be destroyed.
Warm autoimmune hemolytic anemia wAIHA is caused by increased erythrocyte destruction by immunoglobulin G IgG autoantibodies with or without complement activation. To determine whether warm-antibody autoimmune hemolytic anemia AIHA responds to treatment with intravenous gammaglobulin IVGG we conducted separate pilot studies at three institutions enrolling a total of 37 patients. The ability of the bone marrow BM to compensate.
The treatment of warm antibody hemolytic anemia is symptomatic and supportive. Warm autoimmune hemolytic anemia wAIHA is caused by increased erythrocyte destruction by immunoglobulin G IgG autoantibodies with or without complement activation. In addition there is a lack of clinical trials required to refine and.
Relapsehemoglobin11gdLorsymptomatic anemia withongoing evidence of hemolysis. Affected individuals are usually treated with corticosteroid drugs such as prednisone and can usually be well controlled with proper treatment. Warm AIHA can be idiopathic and a treatment plan related to managing anemia.
Other medicines which work on the immune system or rituximab might be used after steroids have been tried. Warm autoimmune hemolytic anemia wAIHA is caused by increased erythrocyte destruction by immunoglobulin G IgG autoantibodies with or without complement activation.